
Because my chemo started just quite soon after I’d had the stoma at the start it was still quite round, and I think probably it’s quite swollen as well for a while until it settles down.
So, it eventually then became oval. So, I have an oval shaped stoma now and when my bags are precut they’re cut into that oval shape.
That changed whilst I was having chemo. The shape of my stoma changed.
I think it most for most people that happens, and it happens within a few months of your stoma being created, but mine did change, so I had to get different bags.
So, after chemo finished, I took chemo for three months and then after that I would say it took a good three to six months after that for my bowel to start to settle down.
I always say to people when anyone asks me, how long does it take for it to get into a regular routine?
You’re told by the surgeons and the stoma nurses will normally tell you it takes about six months for your bowel to settle down. But I would say when chemo comes in between, it took me a good year until I got into a routine, and it does.
I didn’t believe at the start. I didn’t believe it ever would get into any kind of routine. Just thinking this thing is never going to settle down.
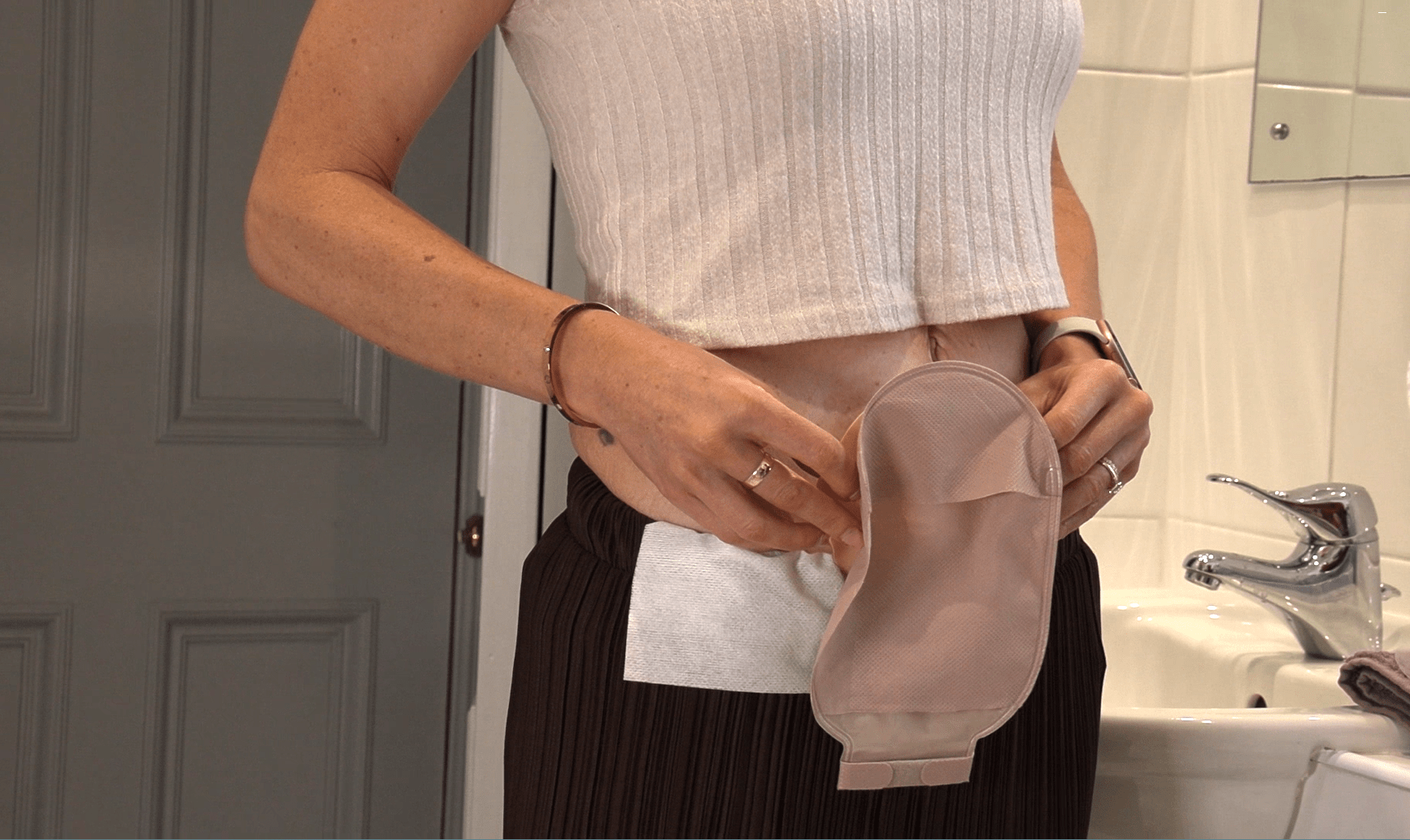
It’s a nightmare and I was changing it, when I came home from hospital, I was changing it five times a day, which at the very beginning that was really horrendous. I came home from hospital with a flat standard bag and it wasn’t, I think because of the velocity of output at the time and your body’s getting used to it that I would say that anybody else, this may not be right for everybody else, but certainly as soon as I discovered a convex bag, it made a big, big difference.
When I came home from hospital, I think because I was just using the standard bag just immediately after getting the stoma, that gave me a lot more leaks. So, like I said, I was changing the bag five times a day and then I had really, really sore skin. That’s when I found out about the barrier wipe and use the barrier wipes.
But my bowel, it did settle down and it did settle down so within a year of me having the operation. It very much settled down and I said, you know, I look back when people say to me is it ever going to settle down, this is a nightmare.
Yes and no, because I was there, but trust me, it really does. It does settle down and it’s now into such a regular routine. Sometimes I even forget I have a stoma.
Practical tips for coping with an irregular routine
Your stoma will change shape and size, tips for managing this:
- Measure your stoma regularly to ensure a secure fit, that the pouch isn’t too loose or too tight.
- Consider a mouldable seal around your stoma as an extra barrier if your pouch is cut inaccurately.
- Your routine may change – don’t worry this is normal, especially as chemotherapy drugs are in your system.
- Your stoma and your body is unique to you, as such it can take a while for your routine to settle but you will get into a rhythm.
- Talk to your stoma care nurse if you are concerned or visit eakin.eu for more advice.

 US
US 




 For five years now I have been working in the maternity setting. Three of these years were spent training on the maternity wards whilst I was reversed, struggling through shifts with loose stools, pain and sore skin. Looking back on my time at university, I often wonder how I managed to get through it. I had my stoma surgery 4 days after qualifying as a midwife.
For five years now I have been working in the maternity setting. Three of these years were spent training on the maternity wards whilst I was reversed, struggling through shifts with loose stools, pain and sore skin. Looking back on my time at university, I often wonder how I managed to get through it. I had my stoma surgery 4 days after qualifying as a midwife.








 Living with a stoma may present its challenges as it has for me, but it doesn’t have to define you or dictate your happiness. By prioritising your mental health, seeking support, and practicing self-care, you can navigate this journey with resilience. Remember, you are not alone.
Living with a stoma may present its challenges as it has for me, but it doesn’t have to define you or dictate your happiness. By prioritising your mental health, seeking support, and practicing self-care, you can navigate this journey with resilience. Remember, you are not alone.