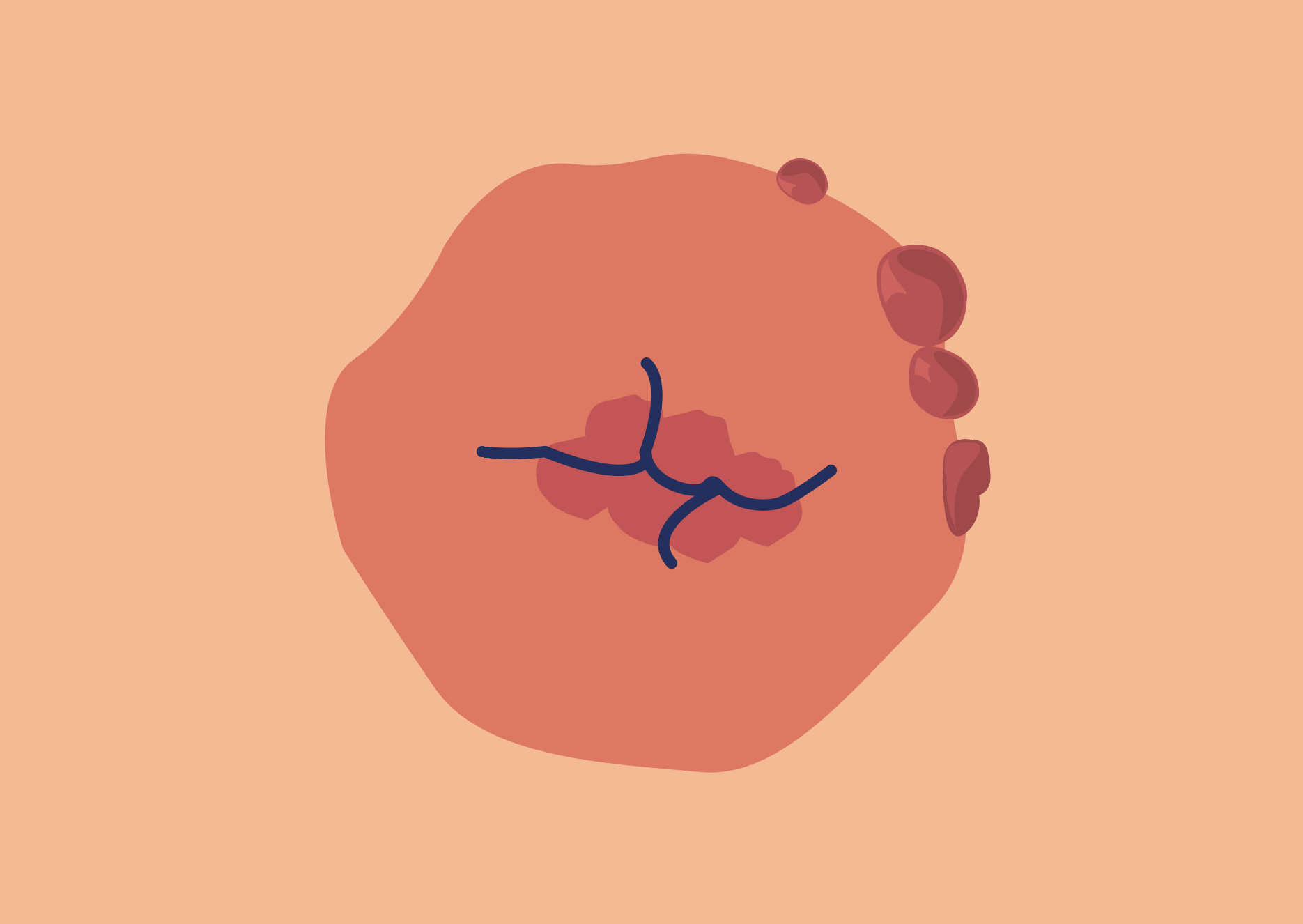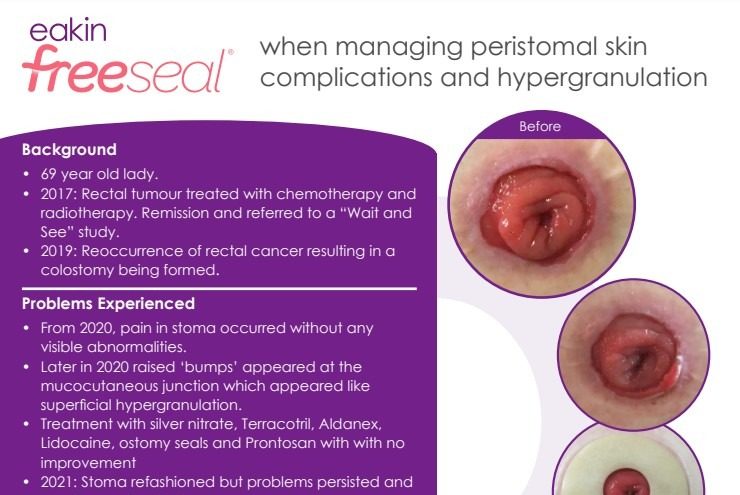
A stoma granuloma is a mass of hypergranulation tissue that forms on or around the stoma due to inflammation when the immune system reacts to/or attempts to contain foreign substances such as suture material. 1,2,3,4
The definitive cause of granulomas is often unknown2
Causative and contributive factors associated with formation of granulomas include:
- Sutures – retained fragments or reaction to suture material.1,2,4
- Repeated trauma from the stomal opening in the pouching system and/or technique in application/removal of the pouching system.2,5
- Chronic irritation from exposure to faecal effluent.2,5,6,7
- Tight clothing or belts that create friction on the mucocutaneous/stomal area.2
- Allergic reaction to pouch material.5
Tips to preventing or managing granulomas
While silver nitrate to cauterise the granulomas is the most recognised treatment option, trying to prevent granulomas occurring or prevent further irritation can be effective.
Some tips to prevent granulomas are as follows:
- Decrease friction and trauma to prevent bleeding.2
- Ensure proper fit of the pouching system; resize the stomal opening for the pouching system as needed and use an ostomy seal.2,3,4
- Apply a barrier paste to the mucocutaneous junction.2
- Avoid tight fitting clothing/belts over the peristomal/stomal area.2
The use of an eakin® seal regularly could help to manage granulomas as shown in a number of case studies. Read below to find out more.
Clinical Resources
Read how eakin® seals can be a successful option in managing granulomas.
Read about the impact of eakin freeseal® on an ostomate’s quality of life who was experiencing peristomal skin complications and hypergranulation.
Read how eakin Cohesive® seals prevented leaks and improved pouch change time on a challenging stoma.
References:
1. Beitz, J. M., & Colwell, J. C. (2014). Stomal and peristomal complications: Prioritizing management approaches in adults. Journal of Wound, Ostomy and Continence Nursing, 41(5), 445–454.
2. Johnson, T. (2010). Problematic stomas…Stoma granulomas. Colostomy Association Tidings Magazine.
3. Salvadalena, G. (2016). Peristomal skin conditions. In J. E. Carmel, J. C. Colwell, & M. T. Goldberg (Eds.) Wound, Ostomy and Continence Nurses Society core curriculum: Ostomy management (pp. 176–190). Philadelphia, PA: Wolters Kluwer.
4. Wound, Ostomy and Continence Nurses Society. (2010). Management of the patient with a fecal ostomy: Best practice guidelines for clinicians. Mt. Laurel, NJ: Author.
5. Dukes, S., Lowther, C., Martin, T., & Osborne, D. (2010). Guidelines for treating stoma granulomas at the mucocutaneous junction. Gastrointestinal Nursing, 8(1), 16–21.
6. Burch, J. (2014). Care of patients with peristomal skin complications. Nursing Standard, 28(37), 51–57. http://dx.doi.org/10.7748/ns.28.37.51.e8317
7. Lyon, C. C., & Beck, M. H. (2012). Chapter 97. Skin problems in ostomates. In L. A. Goldsmith, S. I. Katz, B. A. Gilchrest, A. S. Paller, D. J. Leffell, & K. Wolff (Eds.), Fitzpatrick’s Dermatology in General Medicine, 8e.
Product choice
We have a wide range of pouches, seals and accessories to support your patients following discharge. If you would like samples, please contact your local rep.


 US
US